Asthma is a common illness in New Zealand, 1 in 8 New Zealand children have asthma.
Large numbers of children are still being admitted to hospital with asthma, and some of these will have had a potentially life-threatening asthma attack.
It can be scary when your child or the child you care for has asthma. The good news is that asthma can be well-managed, and your child should be able to live a full and active life.
The Foundation has a range of resources to help parents and caregivers, including
These resources include child-friendly video clips and animations that you and your child can view together to learn more about asthma.
We also have a free, downloadable booklet called Managing Your Child’s Asthma, which is available here.
What is asthma?
People with asthma have sensitive airways. Your child’s sensitive airways may be irritated by a trigger such as pollen, a cold or flu virus, mould, or an emotion (like stress and anxiety). This irritation makes your child’s airways swell up so that it becomes difficult for them to breathe. Find out more about triggers here.
What happens in an asthma attack?
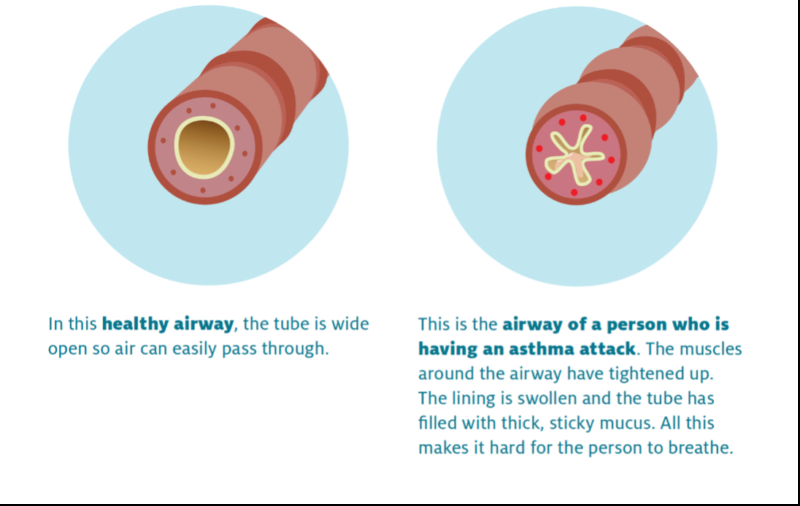
In an asthma attack, which is sometimes called an asthma ‘flare-up’, the bands of muscles around the airways tighten up and narrow. In addition, the inside of the airways becomes inflamed (swollen) and filled with mucus. This makes it difficult for your child to breathe and causes them to cough, wheeze and become breathless.
What are the symptoms of asthma?
There are four main symptoms of asthma:
- Coughing.
- Breathlessness.
- Wheezing.
- A tight feeling in the chest.
Wheezing is a whistling sound that people make when they are trying to breathe through narrowed airways. It is often louder when they are trying to breathe out.
In very young children, who are not able to tell you how they are feeling, look out for the symptoms above and also keep an eye on how tired they are during the day. Children may be more tired than usual if breathing difficulties are keeping them awake at night. In a severe asthma flare-up, you may notice your child’s chest and sides pulling in when they breathe.
Your healthcare practitioner may give you an asthma symptom diary. This is a useful way to understand patterns in your child’s asthma and to identify potential asthma triggers. Read more here.
When and how is asthma diagnosed in children?
Wheeze and coughing in children aged under five years is common and is often triggered by a respiratory viral illness, like a cold, even in children who do not go on to have asthma in later life. By school age, at least half of children who wheeze will have ‘grown out’ of their symptoms. For this reason, healthcare practitioners prefer to wait to diagnose asthma until children have reached school age, and there is evidence of ongoing asthma.
Infrequent pre-school wheeze is a term used to describe a mild wheeze that only affects your child when they have a virus, but otherwise they are wheeze-free. It may be treated with a reliever inhaler.
Pre-school asthma is when your child frequently experiences wheeze (more than every six to eight weeks) or severe flare-ups with viruses, or has other symptoms between viruses or flare- ups, like regular night waking with either a cough or wheeze. If your child responds well to treatment with an inhaled corticosteroid inhaler (like Flixotide®), that is an indication they may have preschool asthma.
Pre-schoolers with wheeze are more likely to go on to have childhood or adult asthma if there is a personal history of eczema, hay fever (allergic rhinitis), or they have a parent with asthma. Learn more about preschool wheeze here.
Unfortunately there is no reliable single ‘gold standard’ diagnostic test for asthma, and diagnosis of asthma may remain uncertain for a period of time. Diagnosis in children is based on looking at the pattern of symptoms, a physical examination, and asking about a history of asthma and allergies in the family. Your healthcare practitioner may trial asthma medicines for a short period of time to monitor a change in symptoms, or they may refer the child to a specialist doctor such as a paediatric respiratory physician.